Flexor Tendon Injuries
What is a flexor tendon?
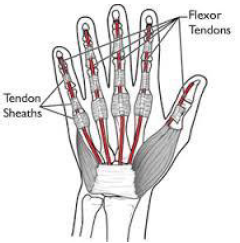
The flexor tendons are the long tendons from the mid-forearm to the fingertip. The muscles originate in the forearm even though their action is in the hand. Each finger has two flexor tendons and the thumb has one. Their actions are complex and injuries to them are devastating.
How does one get a flexor tendon injury?
The most common flexor tendon injury is due to a sharp object (knife, saw, glass). Additionally, one can rupture a tendon when grabbing something or trying to tackle an opponent. The avulsion injury is called a “jersey finger”. This is an avulsion rather than a mid- substance tendon injury. Often this is thought to be a “sprain” as the finger hurts, swells, and can still partially flex.
Why are injuries to flexor tendons so difficult to treat?
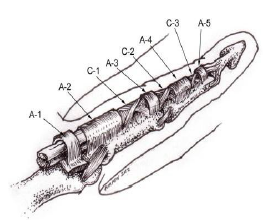
Before the mid-1970s, surgeons would treat all tendon injuries with grafts with minimal success. Very quickly after an injury, the pulley system in the finger will start to ‘shrink’. Also, the injured tendon starts to swell soon after the insult. The result of the swollen tendon and the small pulley make repair after 2 weeks very unlikely. The tendons that are lacerated or injured will heal back to each other when they are repaired. In addition to healing back where they are lacerated, lacerated tendons can to each other (two tendons adherent) as well as to the surrounding tissues. Initial attempts at early repair resulted in a large scar along the tendon with little function.
In the 1970s, a few pioneering surgeons came up with a post-operative protocol using dynamic passive motion. The result was a significant increase in active range of motion and function. This changed the treatment of flexor tendon injuries throughout the world.
How do we repair flexor tendon injuries?
Thousands of papers have been written about operative repair of flexor tendons. Numerous methods and implants have been trialed. The method of choice for lacerations is multiple sutures crossing the gap (the area where tendons are lacerated). The treatment of choice for avulsions is less clear. Tendon fixation to bone with added sutures if possible are used.
We utilize local anesthesia in my repairs of flexor tendons. By allowing the patient to move after the repair in the operating room, the surgeon can tell if the tendon will pass underneath the pulley system. This is very important for rehabilitation.
The role of hand therapy in flexor tendon injuries
Therapy with a Certified Hand Therapist (CHT) is mandatory in anyone with a flexor tendon injury. Often, the patients will be sent to the hand therapist before surgery. Depending on the nature of the injury and the method of the repair, we will start therapy one or two days after surgery. Sometimes we will have to wait if there is a bad wound (table saw, hatchet, etc). The therapist is essential in pushing the patient enough to try and prevent adhesions
Results of flexor tendon repairs
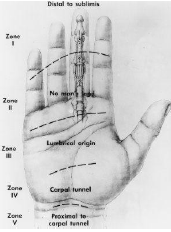
There are many, many factors that affect the outcome of a flexor tendon repair. Most importantly is the age of the patient (young-good, older-not so good), and the type of injury. Very sharp lacerations will have much better results than a table saw injury or a mutilating injury with fractures of the fingers. The location of the laceration in the hand is also very important. The hand has been described in zones. Zone II (from the middle of the palm to the end of the first phalanx) is called “No man’s land”. This is because of such bad results early on with tendon repairs here. This is because of the pulley system. The results are highly dependent on a motivated patient as well.
What is a flexor tenolysis?
If a patient has not regained an adequate range of motion (ROM) after surgery, they can elect to have an additional surgical procedure to ‘loosen’ or break up the scar between the tendons and the surrounding tissue. A patient must have a full passive ROM. This means they must be able to use the other hand to make a fist. It is a common procedure.