Finger Arthritis
What is arthritis?
In general, arthritis is joint destruction. Arthritis can be broken down into 3 broad types:
- Osteoarthritis: By far the most common type of arthritis. It is usually referred to as “wear and tear arthritis”. This is not the case. Osteoarthritis occurs regardless of activity level. It doesn’t matter if you were a pipe fitter or an expert quilter. It is an age-related phenomenon. The smooth layer of cartilage breaks down and does not Some people can get osteoarthritis at a very young age (20-30) whiles others may live into their 90s with no arthritis.
- Inflammatory Arthritis: Less common than OA, inflammatory arthritis is an autoimmune attack on the cells that line the joints and tendons (synovial cells). Inflammatory arthritis includes Rheumatoid Arthritis, Psoriatic Arthritis, Lupus, as well as others. Gout is included in inflammatory arthritis, but it is joint destruction from the deposition of uric acid
- Post Traumatic arthritis: This should be called “wear and tear arthritis.” Any joint that is injured can have cartilage damage. Persistent joint irregularities and/or joints that remain unstable or loose can lose their cartilage.
What kind of arthritis is most common in hands?
Osteoarthritis is by far the most common type of arthritis in the hands and fingers. For some reason, it is more common in women than in men.
What are the common symptoms of finger arthritis?
Surprisingly, the most common symptom of arthritis in the fingers is a painless swelling at the distal interphalangeal joint or the end knuckle of the finger. It is exceptionally common to get osteoarthritis in this joint. It usually doesn’t hurt. It can limit motion. Sometimes arthritis can give rise to mucinous cysts in this joint.
Arthritis will first cause swelling and loss of motion. Pain can result in joint spaces become narrowed or irregular.
Inflammatory arthritis can cause redness and swelling. Sometimes this can be impressive and look like an infection. It can cause a deformity as well
How do we treat finger arthritis?
Activity modification, anti-inflammatory medications, and splinting can help those with minor arthritis. There is nothing to prevent or slow the progression of osteoarthritis or post-traumatic arthritis. If one has inflammatory arthritis, treatment by a rheumatologist is warranted. Some patients can benefit from disease-modifying medications.
Surgical treatment is reserved for those with continued pain. Surgical treatment for finger arthritis will not increase motion or function. It will decrease pain.
What are the surgical treatments for finger arthritis?
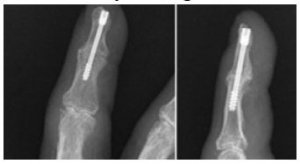
Distal Interphalangeal Joint
Fusion or arthrodesis is the only treatment warranted. Indication for treatment is pain and instability of the joint. We remove what is left of the joint and place a screw to hold it in place. The fusion of the DIP joint is well tolerated and results in excellent pain relief.
Proximal interphalangeal Joint
The PIP joint is very difficult to treat. Recommendations currently are to treat the border digits with fusion (index and small) and middle digits with a silicone arthroplasty. Silicone arthroplasty gives excellent pain relief and modest motion but has little side to side stability. For this reason, the index finger is treated cautiously with a replacement.
Metacarpophalangeal Joint
The MCP joint can do well with silicone replacement or an unconstrained replacement. The most common reason for replacing the MCP is rheumatoid arthritis. By nature, RA causes ligament damage and will require a silicone replacement. This can help to modestly re-align the joints. Osteoarthritis and Post-traumatic arthritis can also be treated with unconstrained joints which theoretically will last longer.
How long to silicone arthroplasties last?
Silicone joint arthroplasty has a high failure rate. One study came up with 50% failure at 10 years.
Unfortunately, we have not developed any better implants than the silicone ones developed in the 1960s by Dr. Swanson. They are just spacers and rely on the patient’s body to form scar tissue to stabilize the joint. Revision surgery for a broken implant is well tolerated with good results.